What is Gastroschisis?
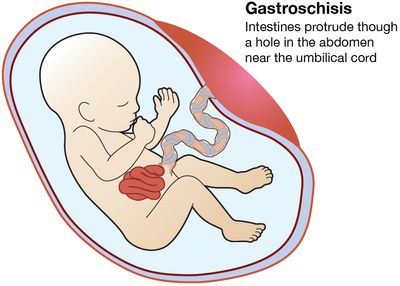
Gastroschisis is an abdominal wall defect like omphalocele in which the anterior abdomen does not close properly allowing the intestines to protrude outside the fetus. The majority of fetuses with this problem are born to mothers in their late teens or early twenties. For some unknown reason, while the fetus is developing, the muscles of the abdominal wall do not form correctly. This allows some of the organs (stomach, intestine) to protrude outside the fetus's body. The organs outside of the fetus's body are floating in the amniotic fluid.
The amount of abdominal contents protruding outside of the fetus varies in each pregnancy. Some are very small (just a few loops of bowel), while others can be quite large and involve most of the intestine and stomach.
What is the outcome for a fetus with gastroschisis?
There is a range of severity for fetuses with gastroschisis that depends entirely on the condition of the intestine. Fortunately, most fetuses with gastroschisis do not have severe damage to the intestine before birth. The relatively normal intestine can be returned to the abdomen and the defect closed in one or two surgical operations shortly after birth. These babies will still be in the intensive care nursery for several weeks before the intestines work well enough to allow feeding and subsequent discharge home. However, the majority of these babies grow up normally .
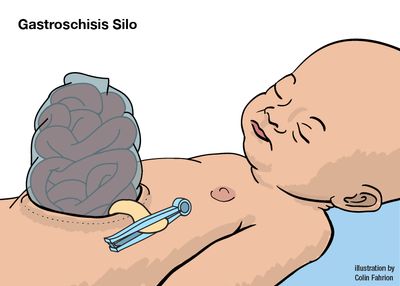
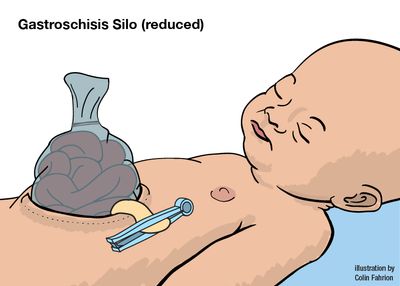
Ten to twenty percent of fetuses with gastroschisis will have significant damage to the intestine that greatly complicates their postnatal course but rarely prevents survival. Babies born with damaged intestine can have a very difficult and prolonged stay in the intensive care nursery. These babies often require several surgical operations to return of the intestine to the abdomen using a plastic silo and eventual closure of the abdominal wall. The bowel can be so damaged that parts of it have to be removed. In the worst case, there may not be enough bowel left to absorb food. The most severely affected babies may not survive, and others may be left with a "short bowel syndrome." At the very least, these babies may require nutritional support in the nursery for many months.
How serious is my fetus’s gastroschisis?
In order to determine the severity of your fetus's condition it is important to gather information from a variety of tests and determine if there are any additional problems. These tests along with expert guidance are important for you to make the best decision about the proper treatment.
This includes:
- The type of defect—distinguishing it from other similar appearing problems.
- The severity of the defect—is your fetus’s defect mild or severe.
- Associated defects—is there another problem or a cluster of problems (syndrome).
Amniocentesis and/or microarray may be necessary for chromosome testing. Sonography is the best imaging tool, but is dependent on the experience and expertise of the physician. Many problems are first detected during routine screening procedures performed in your doctor’s office (amniocentesis, maternal serum screening, routine sonography), but assessment and treatment of gastroschisis before and after birth will require the expertise of a specialized hospital with experience managing complex and rare fetal problems. We can work with your doctor to find a center convenient for you.
A sonogram will accurately diagnose gastroschisis and distinguish it from other similar conditions such as omphalocele. However, the test cannot always tell how severely the bowel damage is. Serial sonograms every few weeks may be necessary to see if the bowel outside the fetus’s body becomes dilated, develops a thick wall, or loses some blood flow.
Since 8 out of 10 fetuses with gastroschisis will not have damaged bowel and will do fine after birth, it is important to be able to identify those 2 fetuses out of the 10 who will have badly damaged bowel and may benefit from fetal intervention before birth. We follow all fetuses with a careful ultrasound examination every week or two to see if we can detect any change in the bowel.
It is very important to plan for delivery at a tertiary center with good neonatology and pediatric surgery for management and repair after birth. While it was originally thought that babies with the bowel on the outside of the body would have to be delivered by Cesarean section, this is not the case and most babies can be delivered vaginally. Good communication between perinatology (obstretricians) and neonatology (pediatricians) is crucial because many of the babies are born slightly premature.
What are my choices during this pregnancy?
It is important to carefully monitor throughout your pregnancy. Additional tests, other than ultrasounds, are not usually recommended, as this is a condition that is not associated with any other birth defect. Rarely, babies can also have bowel obstruction (blockage) as a consequence of the gastroschisis.
Babies with gastroschisis are watched carefully by ultrasound for intrauterine growth retardation (not growing enough while in the womb) and for damage to the intestines. Damage to the intestine can be caused from exposure to the amniotic fluid or by impairment of the blood flow to the exposed intestine.
Since most fetuses with gastroschisis will do well with serial ultrasound observation and preparation for delivery near term at an appropriate hospital, the most important decisions have to do with where the baby will deliver and what team of doctors will look after the baby before and after birth. Your perinatologist (specialized obstetrician) will discuss your delivery plans. It is not necessary to deliver your baby by Cesarean section. Delivering your baby vaginally will not be harmful to you or your baby.
The most important consideration is to be born at the center where the intestines can be immediately covered and kept warm and moist until surgical repair or silo placement. For reasons not immediately understood, mothers with a fetus with gastroschisis will have an increased incidence of preterm labor (delivery prior to 37 weeks). The biggest threat to the baby and to the condition of the intestine is to have to transport the baby to another medical center or in any way delay the repair. Therefore, delivery plans should be coordinated with your neonatologist (specialized pediatrician for newborns) and pediatric surgeon.
What will happen after birth?
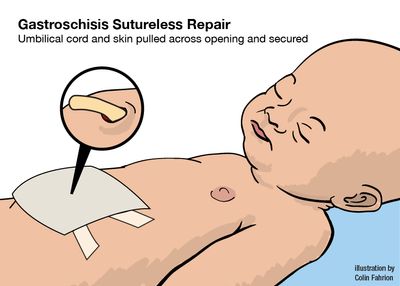
Your baby should be born at a hospital with an Intensive Care Nursery (ICN) and a pediatric surgeon available. Soon after birth, your child will have surgery to close the opening in the abdominal wall and return the organs to the abdomen. The pediatric surgeon attempts to close the opening at the time of surgery, but sometimes this is not possible.
If the gastroschisis is too large, a silo is placed. A silo is a covering placed over the abdominal organs on the outside of the baby. Gradually, the organs are squeezed by hand through the silo into the opening and returned to the body. This method can take up to a week. Babies with gastroschisis can stay in the hospital from 2 weeks to 3-4 months. Because your baby's intestine has been floating in amniotic fluid for months, it is swollen and does not function well. The return of the function of the gastrointestinal tract and the baby's ability to tolerate feedings are two factors which determine the length of stay in the hospital. Babies are discharged from the hospital when they are taking all their feedings by mouth and gaining weight.
After discharge from the hospital, your baby has a small risk for developing bowel obstruction due to scar tissue or a kink in a loop of bowel. Symptoms of bowel obstruction include:
- Bilious (green) vomiting
- A bloated stomach
- No interest in feeding
If any of these symptoms occur, you should contact your pediatrician immediately.
Support Groups & Other Resources
- Avery’s Angels Gastroschisis Foundation — Provides emotional and financial support to families who have babies born with gastroschisis
- March of Dimes — Researchers, volunteers, educators, outreach workers and advocates working together to give all babies a fighting chance
- Birth Defect Research for Children — a parent networking service that connects families who have children with the same birth defects
- Kids Health — doctor-approved health information about children from before birth through adolescence
- CDC - Birth Defects — Dept. of Health & Human Services, Centers for Disease Control and Prevention
- NIH - Office of Rare Diseases — National Inst. of Health - Office of Rare Diseases
- North American Fetal Therapy Network — NAFTNet (the North American Fetal Therapy Network) is a voluntary association of medical centers in the United States and Canada with established expertise in fetal surgery and other forms of multidisciplinary care for complex disorders of the fetus.